Understanding The Differences: Chronotropic Vs Inotropic
In the world of cardiology, understanding the various forces that influence heart function is crucial. Two key terms that often come up are "chronotropic" and "inotropic." While they may sound similar, they refer to different mechanisms that affect the heart's performance. Grasping these concepts is essential for both medical professionals and those interested in cardiovascular health. This article aims to elucidate the distinctions between chronotropic and inotropic effects, their significance, and how they interplay to maintain a healthy heart.
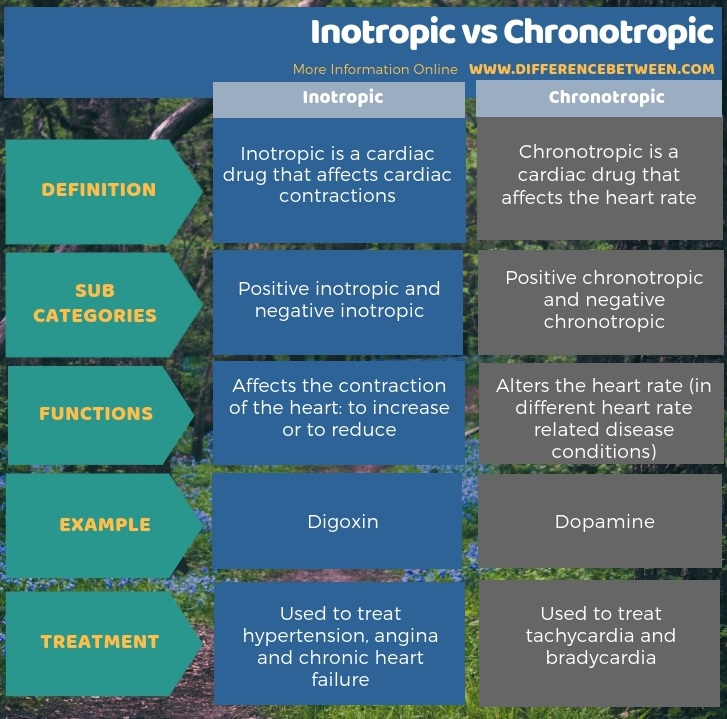
Chronotropic effects pertain to the heart rate, determining how quickly the heart beats, while inotropic effects relate to the strength of the heart's contractions. Understanding these terms not only aids in grasping the fundamentals of cardiac physiology but also provides insights into various medical conditions and treatments. In this article, we will explore the intricacies of these two concepts, shedding light on their roles in heart function, how they can be influenced by external factors, and the implications for patient care.
Whether you're a medical student, a healthcare professional, or simply someone looking to understand more about heart health, this article will guide you through the nuances of chronotropic and inotropic effects. Join us as we delve into the fascinating world of cardiac physiology and uncover the critical differences between these two essential concepts.
What Are Chronotropic Effects?
Chronotropic effects are primarily related to the heart's rhythm and its rate of contraction. The term "chronotropic" comes from the Greek word "chronos," meaning time. Thus, any factor that affects the heart rate is considered chronotropic. These effects are mediated by the autonomic nervous system, which includes:
- Sympathetic Nervous System: This system increases the heart rate by releasing catecholamines such as adrenaline.
- Parasympathetic Nervous System: This promotes a decrease in heart rate through the release of acetylcholine.
The balance between these two systems is crucial for maintaining an appropriate heart rate in response to the body's needs.
What Are Inotropic Effects?
Inotropic effects, on the other hand, refer to the strength of the heart's contractions. The term "inotropic" is derived from the Greek word "inos," meaning muscle. Inotropic agents can either enhance or diminish the force of cardiac contractions. Factors influencing inotropic effects include:
- Calcium Levels: Increased calcium availability enhances the contractility of heart muscle cells.
- Medications: Certain drugs, like digoxin, are used to improve the strength of heart contractions in patients with heart failure.
Understanding inotropic effects is essential for managing various cardiac conditions, particularly those related to heart failure and cardiogenic shock.
How Do Chronotropic and Inotropic Effects Interact?
The interplay between chronotropic and inotropic effects is significant in maintaining cardiovascular health. For instance, during exercise, the heart rate increases (chronotropic effect), and the strength of contractions also elevates (inotropic effect) to supply more oxygenated blood to the muscles. This coordinated response is vital for meeting the body's demands during physical activity.
Can Chronotropic and Inotropic Effects Be Manipulated?
Yes, both chronotropic and inotropic effects can be influenced by various factors, including medications and lifestyle choices. For example:
- Chronotropic Manipulation: Beta-agonists can increase heart rate, while beta-blockers can decrease it.
- Inotropic Manipulation: Positive inotropic agents like dobutamine increase contractility, whereas negative inotropic agents can decrease it.
Understanding how to manipulate these effects is crucial for treating cardiovascular diseases and optimizing heart function.
What Role Do Medications Play in Chronotropic vs Inotropic Effects?
Medications play a pivotal role in managing the chronotropic and inotropic effects on the heart. Healthcare providers often prescribe specific drugs based on a patient's individual needs. For instance:
- Chronotropic Agents: Medications like atropine can increase heart rate by inhibiting the parasympathetic nervous system.
- Inotropic Agents: Drugs such as milrinone can enhance ventricular contractility in patients with heart failure.
These medications are essential tools for clinicians aiming to optimize cardiac function and improve patient outcomes.
How Do Lifestyle Choices Impact Chronotropic and Inotropic Effects?
Lifestyle choices significantly impact both chronotropic and inotropic effects. Factors such as diet, exercise, and stress management can influence heart rate and contractility. For example:
- Exercise: Regular physical activity enhances cardiovascular health by improving heart rate variability and contractile function.
- Diet: A heart-healthy diet rich in fruits, vegetables, and omega-3 fatty acids can optimize cardiac performance.
- Stress Management: Techniques such as yoga and meditation can help lower heart rate and improve overall heart function.
Understanding the impact of lifestyle choices empowers individuals to make informed decisions about their heart health.
Conclusion: Why Understanding Chronotropic vs Inotropic Matters?
Understanding the differences between chronotropic and inotropic effects is essential for anyone interested in cardiac health. These concepts not only help decipher the complexities of heart function but also guide effective interventions for various cardiovascular conditions. Whether through medication or lifestyle modifications, knowledge of these effects allows for better management of heart health, ultimately leading to improved quality of life.
Also Read
Article Recommendations


ncG1vNJzZmivp6x7tMHRr6CvmZynsrS71KuanqtemLyue9OrsJ6bmKR%2BeXvCoamopp%2Bpv7C8yJxkr6tdnruwwNGop6KbXp3Brrg%3D